Abstract
Introduction: Several recent studies have shown the speed and depth of response to tyrosine kinase inhibitor (TKI) treatment to be an important indicator of patient outcomes in chronic myeloid leukaemia (CML) as reviewed in the most recent European evidence based recommendations for CML management (European LeukemiaNet [ELN] 2013; Baccarani et al, 2013). ELN2013 focuses on monitoring of molecular responses, describing "optimal", "warning" and "failure" at specific milestones to guide changes in therapy. An early molecular response (EMR; BCR-ABL1 IS <10%) at 3 months and major molecular response (MMR; BCR-ABL1 IS ≤0.1%) within 12 months are defined as key optimal responses. More recently, the achievement of MR4.5 (BCR-ABL1 IS <0.0032%) has also been associated with improved outcomes (Hehlmann et al ., 2014) and sustained deep molecular response (DMR; BCR-ABL1 IS ≤0.01%) has been suggested as an important requirement for treatment-free remission (NCCN® Guidelines, 2017). Real-world UK data focused on these outcomes are currently lacking, particularly in patients (Pts) switching to second line (2L) treatment. This ongoing study aims to evaluate TKI treatment pathways, monitoring patterns and real-world response rates in UK Pts with CML against ELN2013 to inform future clinical practice. Interim results for the first 126 recruited Pts are presented here.
Methods: TARGET is an observational, retrospective study conducted at 14 UK secondary/tertiary care centres. Data on Pt's characteristics, TKI choice, and molecular responses were collected by review of medical records for adult Pts (≥18 years) with chronic phase CML. Pts first prescribed a TKI between January 2013 and October 2015 were eligible and were required to have at least 6 months follow-up. Data were analysed using descriptive statistics.
Results: At data collection, median follow-up was 21.5 (range 6.0 to 40.5) months. Median age at first TKI was 53.7 (range 18.7 to 86.8) years and 52% Pts were male.
Imatinib was used first line (1L) in 107 (85%) Pts, and a second generation (2G) TKI in 19 (15%) (nilotinib=18, dasatinib=1). During the observation period 52/126 (41%) Pts switched TKI at least once; 29/52 switched early (within 6 [+1] months) and 23/52 switched later. The documented main reason for first switch was resistance (for 36/52) while 16/52 Pts were switched for intolerance (n=13) or other reasons (n=3). The median time to switch was 5.5 (range 0.5 to 34.3) months for Pts switched due to intolerance and 6.7 (range 2.8-16.0) months for resistance.
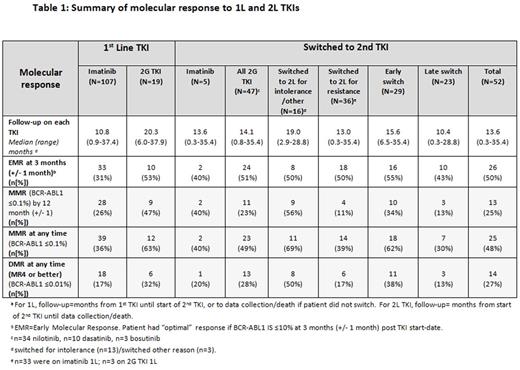
Molecular responses at ELN2013 milestones and rates of EMR, MMR and DMR achieved 1L and 2L during the observation period are shown in Table 1.
In the 52 Pts who switched TKI during the observation period, an ELN 2013 "warning" or "failure" response was observed prior to switch in 19/52 and 21/52 Pts, respectively (note: 4/52 Pts had an "optimal" response and switched for intolerance; 8/52 had no evaluable test at ELN milestone). In the 74 Pts who remained on 1L TKI with no observed switch, 25/74 had a "warning" response and a further 6/74 had a "failure" response at one or more ELN2013 milestones. Rates of MMR and DMR (at any time) for Pts who switched TKI following a prior "warning" or "failure" response (40/52 Pts with median follow-up of 13.6 [range 0.3 to 35.4] months) were 48% (19/40) and 23% (9/40), respectively. In Pts with a "warning" or "failure" response who stayed on 1L TKI (31/74 with median follow-up of 18.0 months [range 6.0 to 37.9]), 29% (9/31) achieved a MMR and 10% (3/31) a DMR.
Conclusions: Interim findings in this real-world UK cohort suggest that a higher proportion of Pts treated with 2G TKI (either 1L or 2L) achieve an EMR, MMR or DMR than Pts treated with imatinib. Early indications suggest that the probability of achieving an optimal response is greater in Pts who switch TKI following an ELN "warning" or "failure" response than those with suboptimal responses who remain on 1L therapy, and that an early switch to 2L TKI may be beneficial. The results also highlight that optimal responses can be achieved even in Pts with prior resistance to 1L. Overall, the results support the use of ELN2013 recommendations to guide TKI management. Further recruitment and extended follow-up are planned to enable more detailed analyses of UK real-world monitoring and management patterns against ELN2013 recommendations and molecular response.
Milojkovic: ARIAD: Consultancy, Honoraria; Novartis: Consultancy, Honoraria; BMS: Consultancy, Honoraria; Pfizer: Consultancy, Honoraria; Incyte: Honoraria, Speakers Bureau. Clark: Novartis: Honoraria, Research Funding; Bristol-Myers Squibb: Honoraria, Research Funding; Pfizer: Honoraria, Research Funding; Ariad Pharmaceuticals: Honoraria. Byrne: Novartis: Consultancy, Speakers Bureau; Ariad Pharmaceuticals: Consultancy, Speakers Bureau; Pfizer: Consultancy, Speakers Bureau; BMS: Consultancy, Speakers Bureau. Raghavan: Novartis: Honoraria; Pfizer: Honoraria. Wandroo: Pfizer: Honoraria; BMS: Honoraria; Bayer: Honoraria. Ali: Novartis: Honoraria; BMS: Honoraria. Ryan: Novartis: Employment; Novartis: Employment. Friedrich: Novartis: Employment. Cross: Novartis: Consultancy, Honoraria, Research Funding, Speakers Bureau; Pfizer: Consultancy, Honoraria, Speakers Bureau; Qiagen: Consultancy, Honoraria; Incyte: Consultancy, Honoraria; Ariad: Consultancy, Honoraria. Mead: Pfizer: Honoraria; Novartis: Honoraria, Research Funding, Speakers Bureau; BMS: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal